The Truth About ‘Gender-Affirming Care’
‘Gender-affirming’ doctors are medicalizing distress in the name of social justice.
Reality’s Last Stand is a reader-supported publication. Please consider becoming a paying subscriber or making a one-time or recurring donation to show your support.
This essay is adapted from Burgo, J. (2024). The medicalization of gender dysphoria. In A. Cantú, E. Maisel, & C. Ruby (Eds.), Institutionalized Madness: The Interplay of Psychiatry and Society’s Institutions (pp. 247–264). Ethics Press.
When I first encountered the apparently benign euphemism “gender-affirming care,” I assumed it meant taking at face value claims to have been “born in the wrong body” made by dysphoric teens and facilitating their access to hormones and surgery.
Working as an expert witness gave me a chance to look “under the hood” of GAC, so to speak, and confirmed my initial impressions. In reviewing years of therapy case notes from affirmative therapists, I found their “biopsychosocial assessments” to be cursory; minimal efforts were made to identify comorbid mental health issues (and only to ensure that they were separately managed), but claims to trans-identification were always validated.
Then I noticed something unusual in these records. When psychotherapists take on new clients, they usually present some form of informed consent/disclosure statement setting forth their policies and procedures; in addition to enumerating rules around payment and cancellation, such disclosure statements will usually describe the practitioner’s theoretical orientation. In reviewing the disclosure statements of affirming therapists, I found references to “anti-oppressive” and “intersectional” psychotherapy. Some therapists described their approach as supportive of BIPOC and other oppressed identities. I heard, for the first time, of “kink positive psychotherapy.”
In preparing to write the chapter from which this essay is adapted, I decided to dig deeper. Among other resources, I reviewed Gender-Affirming Psychiatric Care, a comprehensive guide published in 2023 by the American Psychiatric Association. This book (the “APA Guide”) contains separately authored chapters written by several dozen practitioners in the field. Because a grasp of the ideological language deployed throughout this book is crucial to understanding its argument, I quote extensively from its various chapters rather than summarizing them.
Minority Stress Theory
Nearly all the chapters explore and explain the well-known mental health co-morbidities of trans-identified youth through the identical lens—what is commonly known as the Minority Stress Theory, first propounded by sociologist and public health researcher Ilan H. Meyer (2003). Meyer attempted to account for the higher rates of mental health issues commonly observed within minority groups—particularly, sexual minorities such as lesbians, gay men, and bisexuals—by attributing them to the chronic stress they experience as a result of stigma, prejudice, and discrimination.
Meyer’s Minority Stress Theory has been adapted and expanded by the advocates for GAC to argue that the co-morbid mental health issues commonly observed among gender dysphoric youth are accounted for by the stigma and stress they experience living in a transphobic culture:
Transgender, nonbinary, and/or gender expansive (TNG) people often experience structural and enacted stigma, such as a hostile sociocultural climate, discrimination, rejection, victimization, and nonaffirmation related to their gender identity or expression…Stressors also stem from the general pervasive stigma against TNG people and oppressive systems and cultural norms that seek to invalidate or eliminate them [citations omitted]. These added layers of stressors explain the heightened mental health risks documented among TNG people [citations omitted]. (Matsuno et al., 2023, p. 23)
Most chapters in the APA Guide contain repeated references to this theory; the words “stress” and “stigma” appear dozens of times in reference to an expansive list of oppressed minorities: Two-Spirit People, Asian and Pacific Islander Communities, DoubleQueer (simultaneously neurodiverse and transgender), Disabled, Displaced, and Elderly Transgender people, et cetera.
Taken together, the various chapters in Gender-Affirming Psychiatric Care supercharge Meyer’s careful analysis of the stress experienced by LGB individuals and turn it into a comprehensive account of victimization suffused with postmodern thought and social justice ideology. References to familiar systems of oppression abound—the patriarchy, colonialism, racism, et cetera. To give one impressive example, in critiquing prior studies on “transness”:
[I]t is necessary to approach these studies understanding that the research was conducted under the context emerging from normative cisheteropatriarchal white European colonialist gender norms. As a form of social structure these neuro sexist and racist norms affect the perception of the researcher [citations omitted]. (Sun et al., 2023, p. 34)
Another chapter which discusses the care of transgender people displaced from their countries of origin begins with this sweeping portrait of the forces of oppression experienced by this group: “Structural and infrastructural violence, perpetuated by capitalism, neoliberalism, imperialism, racism, cisgenderism, and heterocentrism, create their international displacement and migration” (Janeway & Anaya, 2023, p. 139). The authors’ critique of oppression is rooted in neo-Marxist thought, with its focus on power dynamics between groups:
Borders are manifestations of the power of citizenship, and they uphold the inequities that create structural and infrastructural determinants of health. From a human rights perspective, clinicians must see borders for what they are: artificial lines drawn through, by, and in support of those in power. (Janeway & Anaya, 2023, pp. 140-141)
Throughout the APA Guide, nearly all the well-known mental health comorbidities demonstrated by gender dysphoric youth are understood and explained through this lens. Anxiety, depression, eating disorders, substance use disorders, and suicidality can all be accounted for by the Minority Stress Theory. And failing to understand how minority stress afflicts TNG people means misapprehending the ultimate source of their comorbid mental health issues: “Without taking these contextual factors into account, clinicians may misattribute mental health issues to a person’s gender experience or pathologize TNG identities” (Matsuno et al., 2023, p. 25).
In the rare event that the authors do not account for co-morbid mental health issues with reference to minority stress, they emphasize that being neurodiverse, for example, should be viewed as a separate and distinct issue and not an impediment to receiving GAC: “Autism alone is insufficient reason to infer incapacity and deny or delay gender-affirming care” (Adams et al., 2023, p. 113). Likewise, “[s]uicidality should not be viewed as a barrier to gender-affirming care when individuals maintain capacity for informed consent” (Joy et al., 2023, p. 265).
Even frank psychosis should not preclude receiving affirmative treatment:
Generally speaking if a person who experiences psychosis is able to draw on their organizational and executive functioning as needed to establish care with a medical provider, seek a referral letter from a health care provider with relevant competencies, obtain medications or surgical dates, and so on, that person's psychotic symptoms are adequately managed to engage in informed consent discussions. (Joy et al., 2023, p. 264)
Nowhere in this volume will you find a single case where the authors consider it valid to question a person’s claimed gender identity. The World Professional Association for Transgender Health (WPATH), in its Standards of Care Edition 8, recommends a thorough mental health evaluation for all patients prior to receiving hormones or surgery (Coleman et al., 2022). But according to APA’s Gender-Affirming Psychiatric Care, such an evaluation should only identify comorbid conditions to ensure that they are adequately managed, not to consider the possibility that they might contribute to a potentially mistaken belief about one’s internal identity.
Not a single example appears of a trans-identification accounted for by one of those comorbid conditions; the possibility that internalized homophobia might drive trans-identification is not even considered. And for the authors of this volume, it would seem that the apparently growing number of detransitioners do not exist. The Index includes a single entry for the phenomenon of detransition, and it refers exclusively to aged TNG adults who “feel pressure to detransition ... or actively conceal their identities out of fear of being misgendered, verbally ridiculed, or abused [citation omitted]” (Dolotina et al., 2023, p. 207), despite the fact that recent research suggests detransition occurs more often for personal reasons such as realizing that their gender dysphoria was caused by other factors, or by internalized homophobia (Littman, 2021; Vandenbussche, 2021).
Gender Dysphoria vs. Gender Incongruence
The APA’s Gender-Affirming Psychiatric Care as a guidebook and GAC as a discipline reject the earlier DSM IV-TR diagnosis of gender identity disorder, which pathologized the condition of cross-gender identification itself (APA, 2000). Because the word disorder implied a type of pathology, the next edition removed it. Diagnostic criteria for the DSM-5 diagnosis of gender dysphoria now speak of a “marked incongruence between one’s experienced/expressed gender and assigned gender” rather than a “strong and persistent cross-gender identification” (APA, 2013).
While the DSM-IV-TR diagnosis refers to “the opposite sex” or “the other sex,” the later version always speaks of “the other gender”; the word sex occurs in the DSM-5 diagnosis only within phrases such as “secondary sex characteristics.” DSM-5 also adds a new criterion: “A strong conviction that one has the typical feelings and reactions of the other gender (or some alternative gender different from one’s assigned gender).” Without explicitly mentioning it, this feature leans heavily upon the belief that everyone has an innate gender identity which may or may not be congruent with one’s “assigned gender.”
“Such incongruence itself is not viewed as a pathological state; only if it causes ‘clinically significant distress or impairment in social, occupational, or other important areas of functioning’ does it merit a diagnosis.”
According to Gender-Affirming Psychiatric Care, the APA undertook this revision of its DSM diagnosis “with the intention of separating objective TNG identity from the objective distress caused by a person’s gender not aligning with societal expectations for their sex assigned at birth [emphasis added]” (Dolotina et al., 2023, p. 202). In other words, one’s internal gender identity must be considered real (an objective fact) and not merely a subjective experience. Further, the subjective experience of distress caused by incongruence is elevated to the same status.
Do the authors not understand the meaning of the word objective?
Once a diagnosis has been given, treatment recommendations and guidelines for practitioners almost always include affirming the person’s gender identity, helping them to understand the explicitly external sources of their distress within a transphobic society, and facilitating access to “life-saving” medical care, including hormones and surgery. Practitioners must also become advocates for their patients and TNG people at large, working to change oppressive social institutions that perpetuate minority stress.
Gender Affirming Care as Advocacy
The APA Guide urges caregivers practicing in this area to educate clients about their oppressed minority status and teach them to recognize external sources of trauma:
Clinicians should be knowledgeable enough to explain (in lay terms) trauma and traumatic stress, the gender minority stress model ... and the ways in which anti-TNG bias, non-affirmation, and intersecting oppression-based stress (e.g., racial trauma) can cause or exacerbate traumatic stress for clients. (Barr et al., 2023, p. 162)
Those who practice GAC should also become social justice advocates themselves, working to change oppressive institutes and attitudes within the culture at large:
Mental health clinician advocacy is a critical component of trauma-informed care and should address power asymmetry; protect and enforce human rights; and foster social justice through empowerment … Indeed, without advocacy, clinicians are endorsing the silence, violence, and injustice that have contributed to clients’ traumatic stress… (Barr et al., 2023, p. 163)
Even when ostensibly performing a more traditional psychotherapeutic role, practitioners must never lose sight of their role as advocates for social change:
An exclusive focus on coping and social support in the context of oppression frames psychological distress as what must be changed rather than the systems of oppression that give rise to that distress … Distress alleviation is fine, but coping and social support by themselves are unlikely to lead to changes in the oppressive systems that give rise to factors causing distress … or to curtail future experiences of gender minority distress. (Noyola et al., 2023, p. 188)
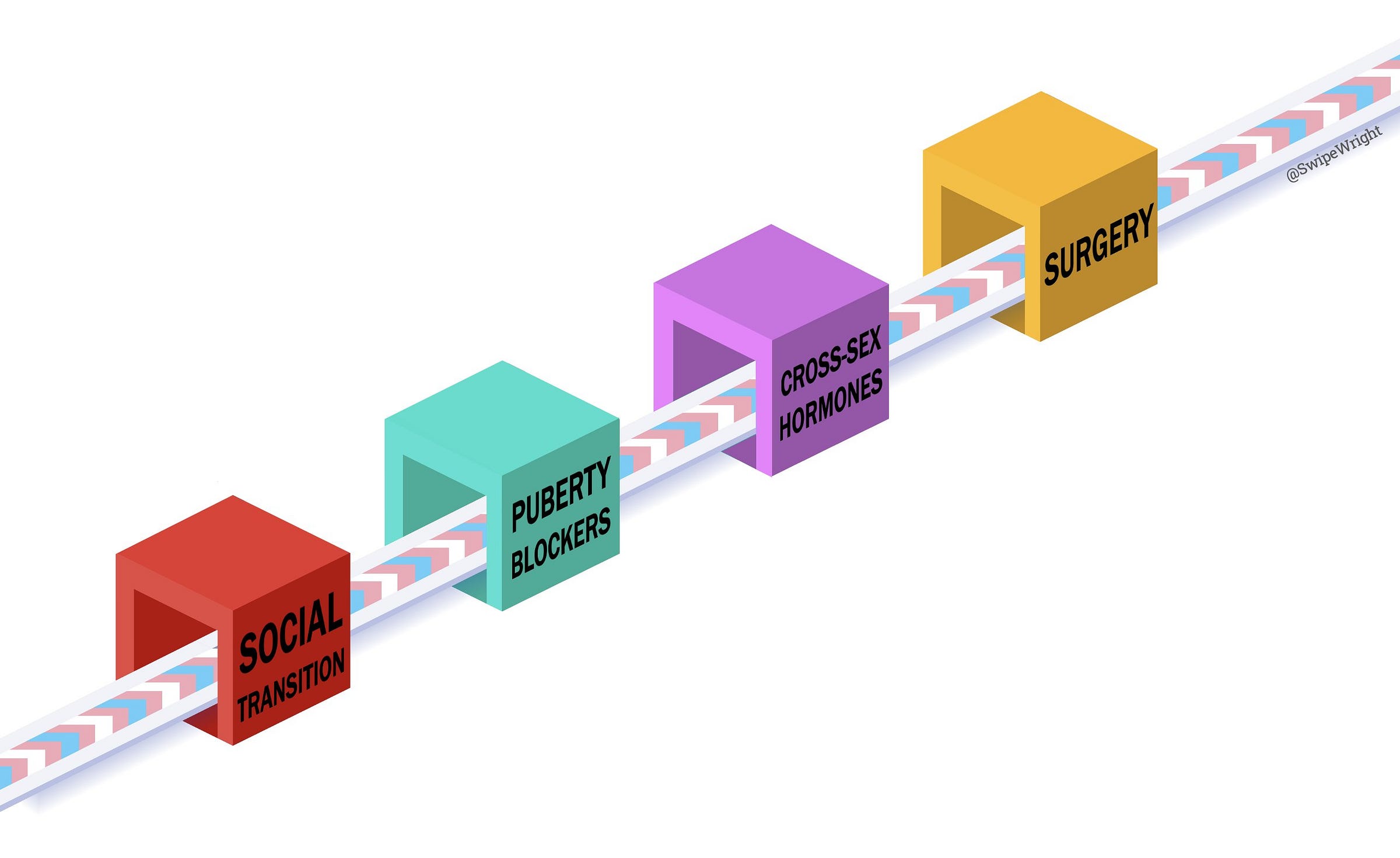
The Medical Treatment of Gender Dysphoria
The ultimate conclusion readers will draw is that medicalization is the only acceptable and ethical form of treatment, and that practitioners must do everything within their power to facilitate access to gender-affirming medical care for their TNG clients. A two-page chart presents a list of “Physical presentations and sources of distress of gender dysphoria” including distress around menses, the chest/breasts, hips, face, stomach, and genitals (Goetz, & Silverstein, 2023, pp. 217–218). Nearly all recommended remedies (“Clinician Opportunities”) involve medicalization: optimize hormone treatments, refer for top surgery and/or hysterectomy, refer for facial masculinization or feminization surgery, refer for liposuction, refer for “genital gender-affirming surgery,” and so on.
In short, GAC has virtually nothing to do with traditional psychotherapeutic technique or goals. It begins by presenting the theory of gender identity as fact, then proceeds to psychoeducation for clients in Minority Stress Theory as applied to trans identity. It relegates comorbid mental health conditions to their own separate silos and ends with a referral for hormones and/or surgery, in effect continuing the medicalization of human distress.
As a quasi-spiritual belief system, it elevates subjective experience to the status of objective fact. Rooted in neo-Marxist thought and framed in the language of social justice ideology, it treats access to affirmative medical care as a civil rights issue and views any other lens through which to understand and treat gender dysphoria as an exercise of power by a transphobic culture attempting to enforce its imperialist, racist, and heterocentrist norms upon an oppressed minority.
You made it to the end! You must have enjoyed the article. If so, please consider upgrading to a paid subscription or making a recurring or one-time donation below. Reality’s Last Stand is a reader-supported publication, and your help is greatly appreciated.









Excellent piece.
I have long believed that the psychiatric profession has abrogated its responsibility to bring critical thinking to this topic. Why does the gender dysphoria delusion get the special status of a "normal variation". The only thing that is aberrant is the "distress", and that is why the breasts are removed. Right?
(speaking as a doctor and surgeon) so basically the working theory is, 100% of people, including children, who experience significant “gender dysphoria” 1) their beliefs are always true and in their own best interest. and 2) the treatment is always affirmation of this belief and treatment with medication and surgery. and 0% of these people could possibly be mistaken and/or better treated with therapy to accept the body they were born in, their biological sex (and still live and express themselves however they feel). there is literally no psychological state known to man for which this could possibly be true. and the fact that alternative treatments are not being actively pursued and studied tells one all they need to know about this as ideology, dogma, agenda, not science. this is both tragic and evil.